THE DURYSTA® DIFFERENCE:

Reliable, non-incisional
IOP control*

Studied in patients with mild
OAG and OHT1,2

Bypasses the ocular surface to
directly deliver medication1,†
*Primary efficacy endpoint: The study eye IOP at each hour was evaluated (Hours 0 and 2) at Weeks 2, 6, and 12.1
†DURYSTA® demonstrated a mean IOP reduction of approximately 5 to 8 mm Hg over 15 weeks in patients with a mean baseline IOP of 24.5 mm Hg.1
ONE BIODEGRADABLE IMPLANT—
AROUND-THE-CLOCK MEDICATION FOR SEVERAL MONTHS

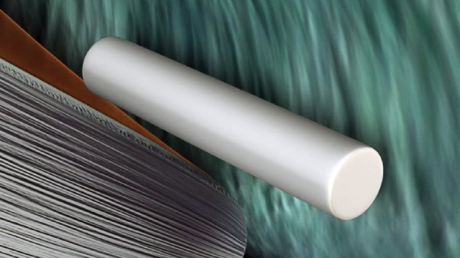

DURYSTA® implant
DURYSTA® is a dissolvable bimatoprost implant that can be administered in your office or at the ASC. DURYSTA® is placed directly in the eye and slowly degrades into lactic acid and glycolic acid.1
Learn how DURYSTA®
works for several
months

Discover the pivotal
data behind this
therapy
Where DURYSTA®
may fit in the
treatment paradigm

Access DURYSTA®
resources for your
practice

Start the DURYSTA®
ordering process
today
IOP = intraocular pressure; ASC = ambulatory surgery center.
References: 1. DURYSTA® Prescribing Information. 2. Medeiros FA, Sheybani A, Shah MM, et al. Single administration of intracameral bimatoprost implant 10 μg in patients with open-angle glaucoma or ocular hypertension. Ophthalmol Ther. 2022;11(4):1517-1537. doi:10.1007/s40123-022-00527-6.


